Consultants recommend Ely hospital regain ownership, operation
After nearly two decades utilizing a different approach, local ambulance service could very well return to its roots.
Consultants retained by Ely-Bloomenson Community Hospital recommend that the hospital resume ownership and operation of the regional ambulance service, which in recent years has been stymied both by financial losses and struggles with attracting and retaining personnel.
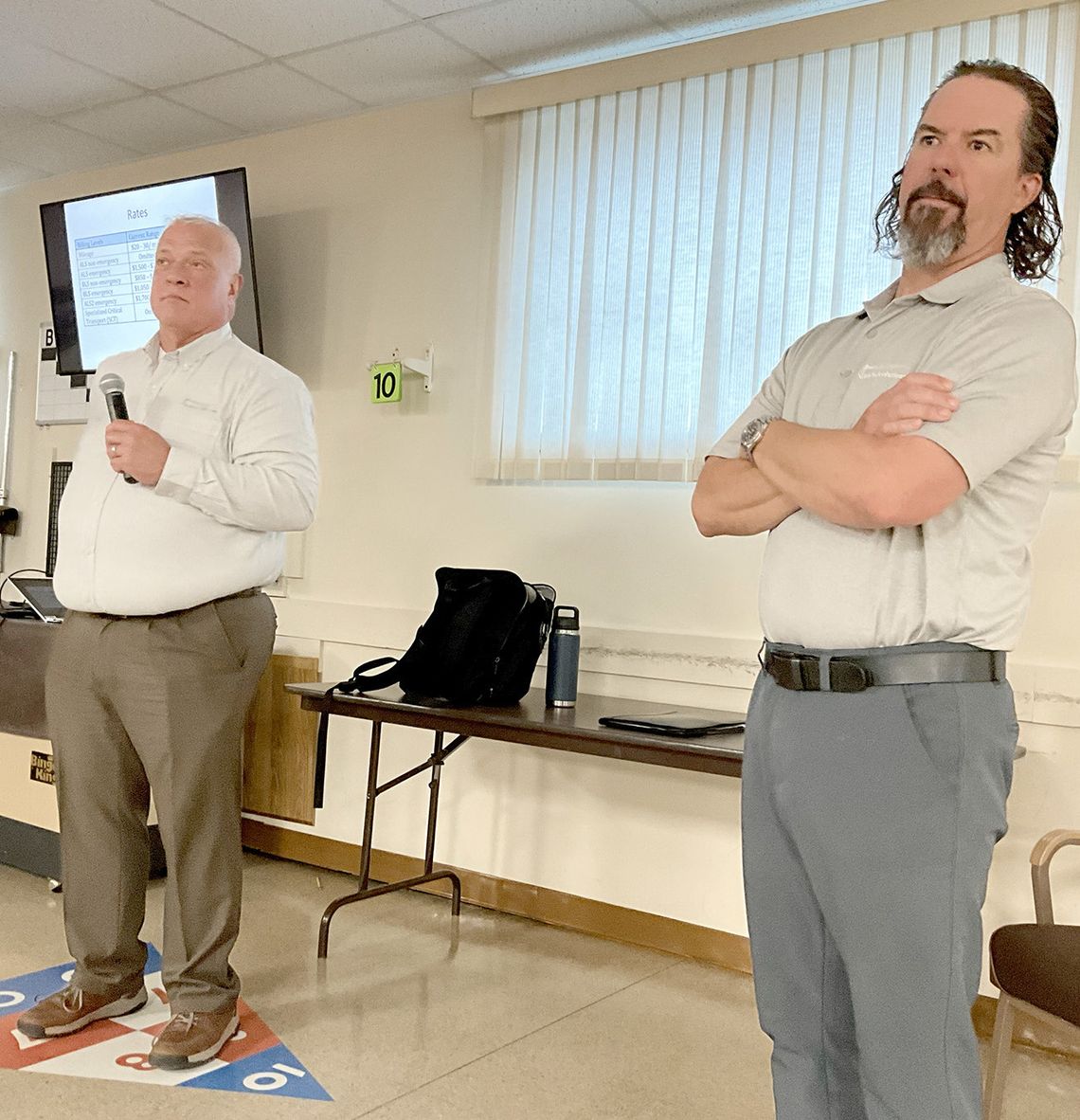
The recommendation was made public June 13, during a public meeting attended by hospital, emergency services and local government officials at the Ely Senior Center.
Representatives of Safe-Tech Solutions, the firm that completed a comprehensive review of regional ambulance operations, conceded their recommendation needs “buy-in” by local leaders, but they maintained it’s the best option given the hospital’s standing as a critical access facility.
“Because you have a hospital where you have it and it’s critical access, it could be a game changer when it comes to reimbursement,” said SafeTech’s Ben Wasmund, one of two presenters at the meeting.
Medicare reimbursements under the current structure can be as small as 30 cents on the dollar and encompass up to two-thirds of the runs made by area ambulance services, but those reimbursements climb to as much as 101 percent should billing originate from a critical access hospital such as EBCH.
That makes a world of difference in financial models, including one calling for as many as four fully-staffed ambulances in the Ely, Babbitt, and Tower areas and an operation with more than 30 full-time personnel.
“That one will cover the expenses and potentially have some net revenue that go for reserves and capital expenses,” said Wasmund. “If you do any of the other models without changing the structure you pretty much show a loss. It can’t be done unless it’s under the hospital.”
EBCH board members heard a similar presentation last month and opted to share the results publicly at a meeting attended by representatives of local governments, who form a joint powers board that provides funding to the private Ely Area Ambulance Service. The EAAS was also represented at the meeting, as were staff from the Tower ambulance service.
The EAAS was formed in the late-2000s, after the Ely hospital relinquished ownership of the ambulance services - in large part because of financial implications and Medicare reimbursement policies then.
There was little give and take at the meeting, which attracted about 50 people, and local governments, the respective ambulance services and EBCH have further time to weigh the recommendations and determine the next steps.
Wasmund said the groups could opt to maintain the status quo and added that the study found “confrontation” and “tenseness” between the entities.
But Ely’s ambulance service has needed additional subsidies from local governments to stay afloat. Legislation passed this year that provides additional monies is only temporary and little more than a band-aid, according to Wasmund.
“Your systems today are at a bit of a dangerous level,” he said. “Many of them are really struggling with staffing (and) some of them are struggling financially.”
The study began with interviews of key stakeholders and a look at data, which showed a combined 1,620 ambulance calls per year in the Ely, Babbitt and Tower areas.
Wasmund noted that the study found that staffing challenges have taken a chunk out of a key revenue source, interfacility hospital transfers.
“How do we get somebody to Duluth if they need to get to Duluth?” asked Wasmund. “That’s one of the challenges.”
Currently, 11 percent of interfacility ambulance calls are unable to be made because of staffing shortages. Those transfers end up going by personal vehicle.
Wasmund said SafeTech’s goal was to develop “what a system could look like in this area. The idea was if there were to be a system-wide approach what could it look like. How can you in your area have an EMS system that’s reliable, viable, sustainable and equitable?”
The study found that a system-wide approach would reduce duplication of services, and that expenses continue to rise while reimbursements are falling, and that relying on volunteers or part-time staff to operate ambulance services is unlikely to be a reliable model moving forwards.
They also found that a new system/operator would need all of the call volume and all of the interfacility transports to maximize revenue, and that even with that set-up, some public subsidy may eventually be needed SafeTech looked at models including those that mirrored or closely mirrored the status quo, or systems that put two staffed ambulances in Ely, and relied either on staffed or volunteer models in Babbitt and Tower, and those with a quick response ALS vehicle that could move between the communities.
The cost-based reimbursement model, which would apply only under hospital ownership, quickly rose to the top.
“It changes everything when you talk about paying for the system,” said Wasmund.
SafeTech’s Tom Fennell looked at the financial implications of the various models and noted the billing challenges that the EAAS and other ambulance non-profits face.
“When you’re billing $1,200 and getting $257, these programs are designed for helping people on fixed incomes but you’re getting cents on the dollar,” he said.
The system recommended by SafeTech would put fulltime staff on ambulance duty, with two staffed ambulances in Ely and one each in Babbitt and Tower, with wages of $19.25 per hour for EMTs and $25.75 for paramedics, with additional funds set aside for benefits.
Placing the license under the umbrella of EBCH would allow the ambulance to have satellite stations in Tower and Babbitt, and the various ambulances would cover for the other in the event of transfers.
Fennell said EBCH has the infrastructure to handle human resources, billing and other administration, and said the compensation model would help in attracting staff.
It would mark an upgrade in service in Babbitt and Tower, where ambulance operations do not have fulltime staff.
The switch may also come with some up-front costs, including the securing of crew accommodations in Tower.
The model calls for roughly 8.4 full-time equivalent personnel for each of four ambulance vehicles that would be in operation in the area.
While some of the other models considered come with smaller overall expenditures, none qualify for the larger reimbursements that would come if EBCH took over ownership.
“If it’s not owned by the hospital, you lose the cost reimbursement, you lose the hospital infrastructure,” said Fennell.
The consultants said leadership is important as local officials ponder what to do next.
“We understand there’s challenges to that,” said Wasmun. “There’s pride in Tower being on the side of the ambulance. Same with Babbitt. We’re talking about changing that and giving up power and control, and we realize it’s not a simple thing to ask.”
The consultants also indicated that should even one entity opt against a new system, the financial picture would change accordingly.
“You as a community have to get behind this and say this is something you want,” said Fennell. “Leadership is something of utmost importance for it to be successful.”
Local governments have pumped funding into the EAAS to keep it viable, and the service stands to get better than $265,000 in additional state funds as a result of legislation passed last month.
But those are likely to be only short-term fixes given ongoing challenges including lagging reimbursement rates and higher personnel costs.
“That’s not going to help two, three, four years down the road,” said Wasmund.
Instead, the information will be presented to allow the various entities represented at the meeting to take time discuss and process the information independently.
The ambulance crisis across rural Minnesota has captured the attention of area legislators State Sen. Grand Hauschild (D-Hermantown) and State Rep. Roger Skraba (R-Ely), who were both present in Hoyt Lakes May 23 when Gov. Tim Walz came to the Iron Range to sign legislation that pumped about $30 million into local ambulance services.
Hauschild, Skraba and State Rep. Dave Lislegard (D-Aurora) also all took part in meetings convened by an EMS Task Force, which highlighted the challenges facing rural ambulance service.
Leaders have also engaged representatives at the federal level, including U.S. Sen. Tina Smith (D), U.S. Sen. Amy Klobuchar (D) and U.S. Rep. Pete Stauber (R).